Citizen health innovators: Exploring stories of modern health
Everyday citizens are becoming empowered to contribute to modern medical science.
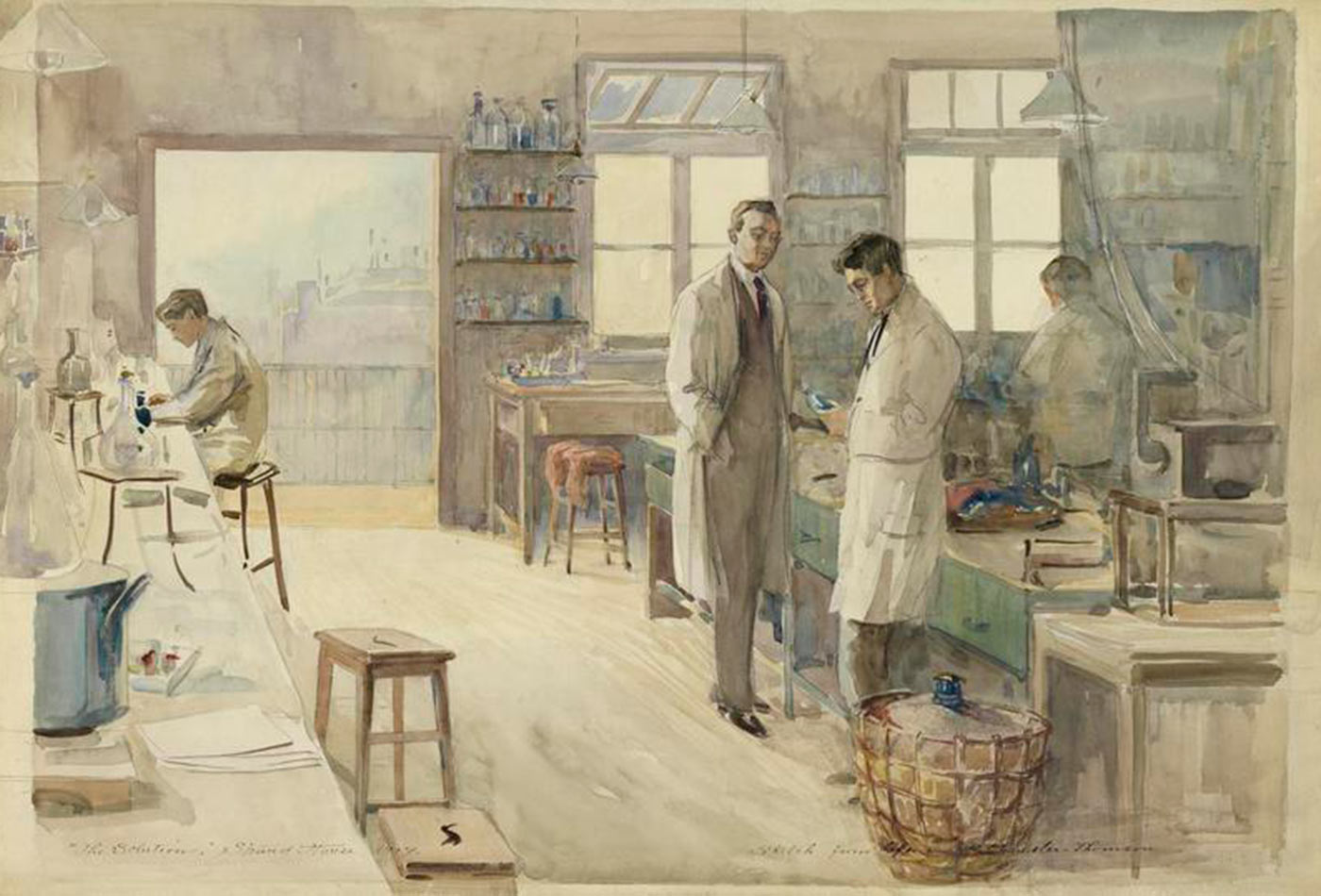 The Laboratory at Strand House, Portugal Street, London, 1917. (source: The Imperial War Museum on Wikimedia Commons)
The Laboratory at Strand House, Portugal Street, London, 1917. (source: The Imperial War Museum on Wikimedia Commons)
From the Mylan EpiPen pricing scandal, to the whistleblower story that crashed the blood-testing startup Theranos, among many Americans, there is a growing public distrust in governance over the biomedical enterprise and there are questions being raised about who gets access to cutting-edge sophisticated drugs and therapies.
At the same time, there’s a parallel story brewing about citizens who decide not to wait to shape their own medical future. One of them is Tal Golesworthy, a bright and resolved engineer who, suffering from a genetic disease that damages his heart, designed a surgical device that would save him and other patients from a more risky procedure. Dana Lewis, a digital communication specialist suffering from Type 1 diabetes, created an artificial pancreas based on an algorithm that calculates the need for insulin based on a patient’s blood sugar levels. And to find a cure for their daughters suffering of the rare Batten disease, a couple raised millions on a crowdfunding platform to hire their own research team. While these individuals and other communities are reshaping their involvement in health research and practice, they are raising new ethical, safety, and governance issues for policymakers, practitioners, and patients.
This participatory turn has no official name. Some say “patient-led” or even “patient-powered” research, others “DIY health.” We call them citizen health innovators and have begun mapping their emergence and exploring their stories, as well as the ethical and regulatory landscape that surrounds them, with funding from the Robert Wood Johnson Foundation (Map and Website). But how did we get there? What enabled this new societal phenomenon to arise? We identified the convergence of three factors that contributed to a form of democratization in health research and practice: vanishing barriers to entry, the rise of and access to personal genomic data, and the emergence of crowdfunding platforms.
First, the barriers to entry to an array of genetic and biotech techniques have decreased to a considerable extent through PCR machines, gene-editing test kits, and portable genetic sequencers. There is also now the possibility to sequence a genome for about $1,000. Second, biomedical research is increasingly relying on personal genomic data to tailor diagnostics and therapies to groups of patients, creating the incentives for individuals to resort to personal genomics and learn about their own genetic blueprint. The third and possibly most important factor which contributes to this participatory turn is the access to financial backing that citizens recently gained through crowdfunding platforms. After raising about $2,642,000 on experiment.com, the parents of Charlotte and Gwenyth Gray decided to hire their own research team to accelerate research in three promising treatment options for Batten disease: gene therapy, cellular therapy, and small molecular therapy.
While the convergence of these factors is not necessarily a silver bullet to a cure, it does enable us to imagine one. Which begs the questions, what if it works? And what should the role of government be in these new endeavors? After all, some of these are health conditions and diseases that the traditional research communities have largely ignored or treatments that people cannot afford.
Several governance issues lurk in the background. Compared to standard National Institute of Health (NIH) grants, which can take up to a year to get funded, crowdfunded research can begin in as little as 30 days from when a project is launched on a site. There is currently no official safety and ethical oversight, or a traditional peer-reviewed system that accompanies these proposals, raising complex questions for crowdfunding platforms to tackle. Who’s liable when it comes to delivering on the results promised in the funding pitches? Is there a responsibility for the crowdfunding platform to properly vet projects, similar to the NIH peer-reviewed process? Or are they simply a conduit to pass money through with no responsibility, similar to Western Union or bitcoin?
What about the quality of data coming from patient-powered health research? How will traditional academic journals and government agencies assess the data derived from crowdfunded studies that may not have applied NIH rules for health research? If journals and agencies reject such data, does it even matter if the protocols established to produce the treatments and medical devices are accessible to other ends users? Facing regulatory uncertainty, patient innovators might not overcome this “chill factor,” a phenomenon described by DIY inventors as the fear to confront regulators by sharing the recipe for a new invention.
The press might cover the few memorable cases of patients who self-experimented with unregulated gene therapy treatments. But those are not common practice. As shown on this map, patient innovators address crucial user-centered issues with their designs often vetted by peers and doctors who have become collaborators in their shared innovation journey. Nonetheless, we argue that it is important to think creatively about how to help patient innovators share their data, evidences, tacit knowledge, value trade-offs, and ethical concerns in ongoing conversations with regulators and society at large.
We, as a society, are at a tipping point. We could build a new innovation ecosystem that ensures safe and responsible citizens’ participation in health research, or we could drive these emerging communities of innovators at the margins, underground or out of existence. What can patients teach us about user-centered research and design? How can regulators help them embed responsible governance mechanisms into their endeavor? How, in turn, can this culture of responsibility confer legitimacy to patient-powered health research?
The goal of the Citizen Health Innovators Project is to develop engagement channels with innovators, patients, ethicists, and regulators to design adaptive oversight tools that will foster a culture of empowerment and responsibility. We envision building an open and distributed health innovation ecosystem that empowers patients through tailored inventions and is seconded by adaptive regulatory institutions. This effort to provide patient-led research with more legitimacy is a collective endeavor that needs new practices. Will you join us?
Support for the Citizen Health Innovators Project is provided by a grant from the Robert Wood Johnson Foundation. The views expressed here do not necessarily reflect the views of the foundation.
