Bioprinting: From a DIY revolution to patients
Bioprinting, a technology that emerged from open source communities, has the potential to improve medical science.
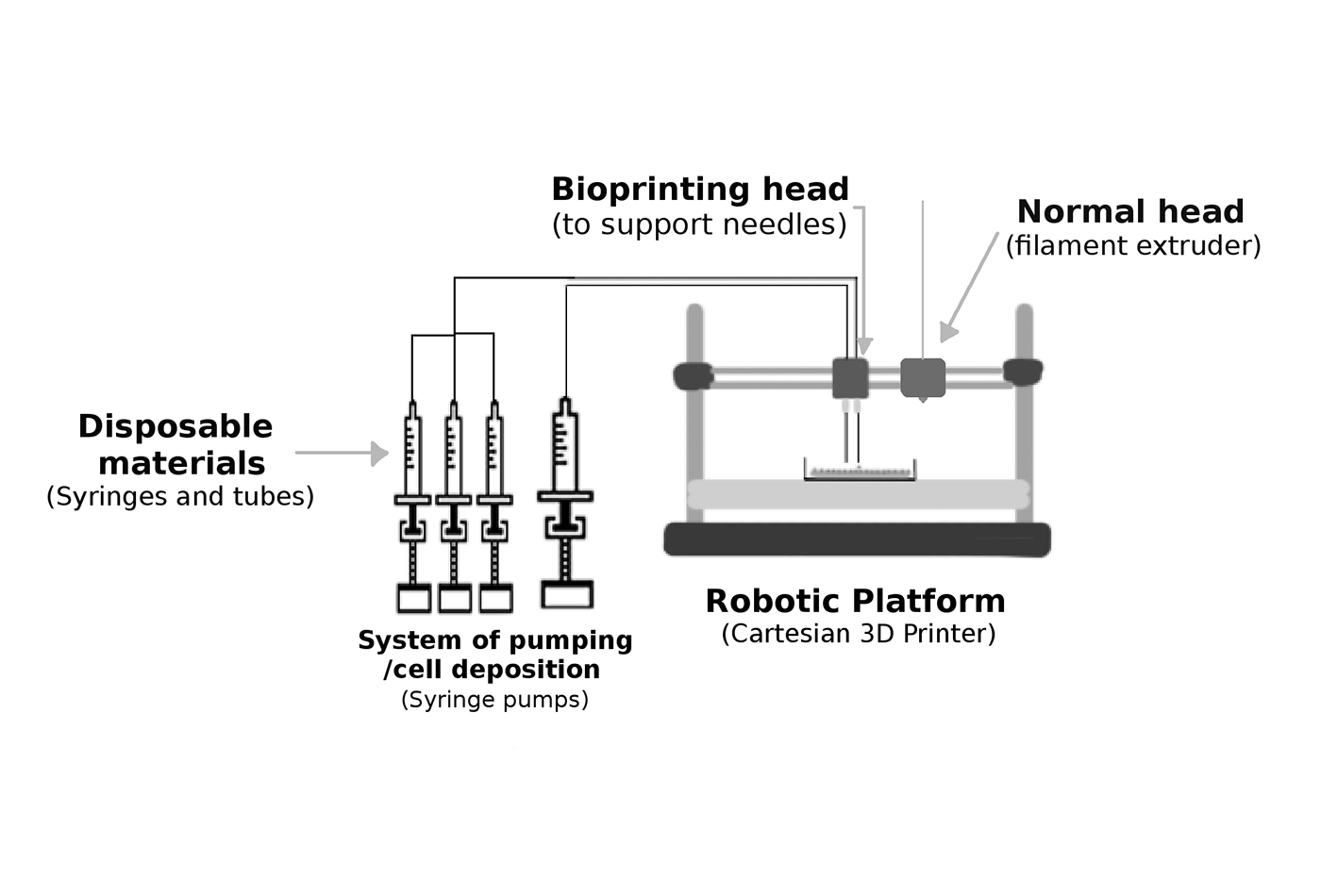 Basic elements of a bioprinter. Image reused with modifications. (source: Nieves Cubo Mateo, used with permission)
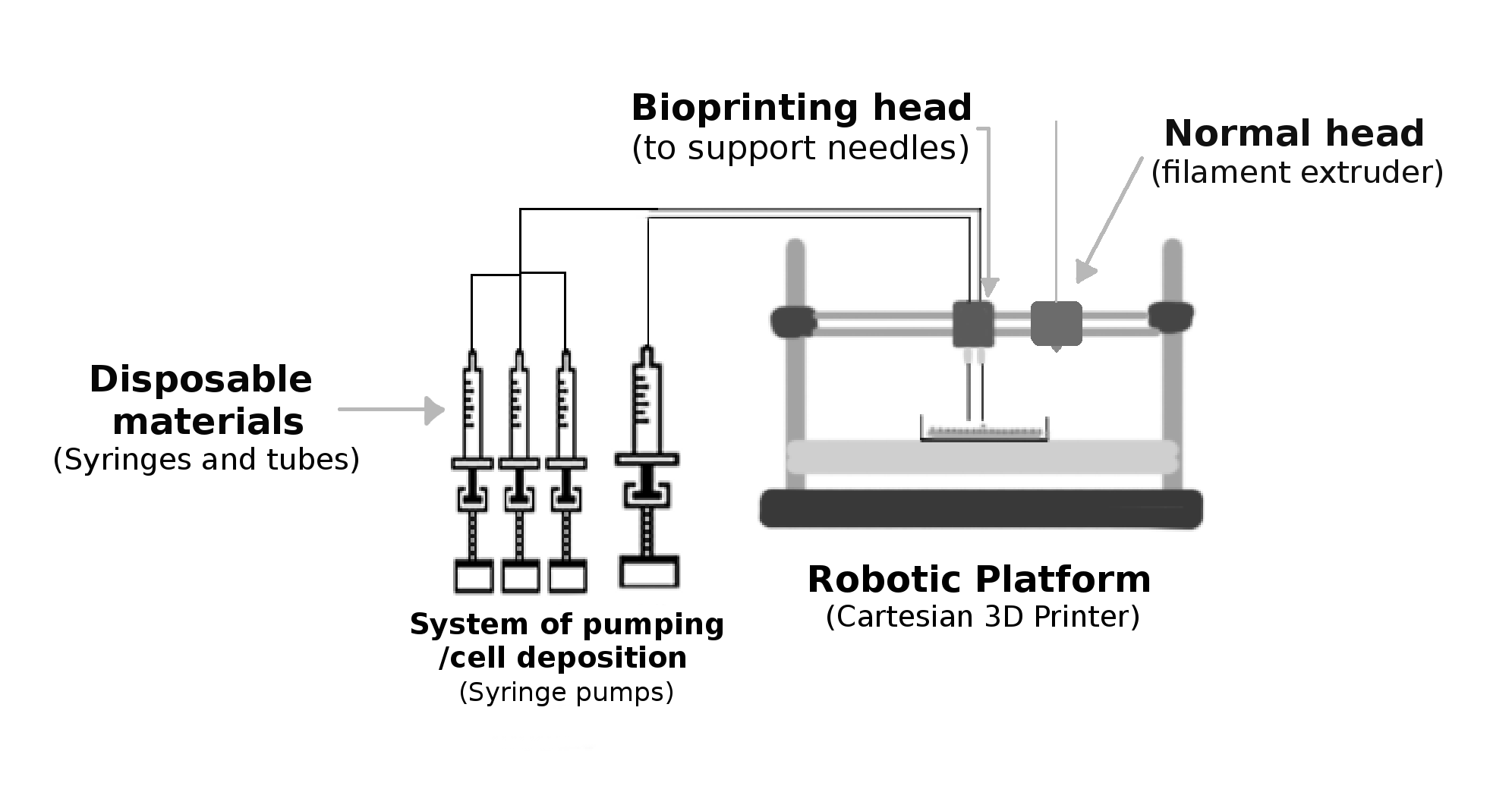
Basic elements of a bioprinter. Image reused with modifications. (source: Nieves Cubo Mateo, used with permission)
Advances in health concern us all. It is important to keep in mind that at the end of research and development, there are patients who need these advances to recover and survive. That’s why when a new technology that promises to shorten transplant waiting lists is released, it should reach the entire world. To reach this aim, researchers will have to work together to innovate low-cost and higher throughput technologies.
Openbioprinting.org does just that. The initiative allows bioprinting developers to discuss, collaborate on, and share pieces, protocols, and research results from anywhere in the world.
Most of the technologies used in bioprinting come from the free movement that emerged after the expiration of the first 3D printers patents (Figure 1-1). These developments have Creative Commons licenses, in many cases SA (Share-Alike). That’s why when we look for information about how to make bioprinters, what we find are several initiatives belonging to the field of DIYbio, where researchers and citizen scientists together develop new methods and materials to be used in bioprinting (not only for medical applications, but also for arts, basic research, and ecology printing with algae and bacteria).

It’s trendy to use terms like DIY (Do It Yourself), or the analog one when referring to a group of people (DIWO, Do It With Others). However, these practices have been done for many years in scientific environments where the necessary machines did not exist or existed but were beyond the reach of researchers for economic reasons.
This is how our project to create human tissue began. Starting with our own 3D designs and taking parts from open source projects, such as the Printrbot, from pages where some people had voluntarily uploaded their designs, like Thingiverse. The first 3D bioprinter we developed was able to print tissues, as human skin, without causing any damage to the cells or to the other biological components used. For more information about this work, please look at the published article on Biofabrication.1
These kinds of projects show that it is possible to do an investigation, despite having few resources, when people collaborate and share their knowledge for a common, greater good. When the purpose of an investigation is to improve the life of a patient, everybody has to push in the same direction.
The most important fact about bioprinting is that it allows researchers to build personalized tissues with the patient’s own cells, reducing the probability of rejection and enabling a better recovery. With this technology, we are not just replacing a part of the body but regenerating it, so at the end of the process there is no artificial prosthesis inside the patient, but instead human tissues.
Another important issue is that if we are able to emulate these tissues in vitro (at the lab), we could use them as alternative methods for animal testing.
How to Build a Bioprinter2
First of all, we will be working with cells either from human or animal origins, so we will need to adapt normal printers in order to avoid any damage or contamination. The normal 3D printing techniques use high temperatures (from 60 to 300º C) to change the state of the plastic and to build a layer by layer structure in a very controlled pattern. However, we will not be able to handle such temperatures with cells, so new techniques and technologies are required.
Knowing this, these are the basic elements that anyone will need to build a bioprinter (Figure 1-2):
- A robotic platform that moves in three dimensions within a certain space. It can be a Cartesian configuration like in 3D printers, or robotic arms like those used in automation processes (SCARA, spherical, polar, etc).
- A system of pumping/cell deposition, to infuse cells. It can also be used to deposit other liquid or gel materials. The commonly used systems are peristaltic pumps, piezoelectric systems, and syringe-pumps.
- A support that would replace the conventional head extruder in the printer, as we do not want to fry cells at temperatures over their survival one, nor contaminate them with the mechanism.
- An extra conventional head (optional) to work with biocompatible thermoplastics (PCL, PLA, PGA, etc.) that can be used to reinforce the cell matrices, without damaging the cells with these high temperatures.
- A disinfection or decontamination system for items to be reused.
- Single-use (disposable) materials that will be in direct contact with the cells of each patient.
Again, when working with human cells, we must offer them an environment in which they can live, nourish themselves, and breathe. In addition, when depositing them, there are some factors that can be critical in their viability (survival), such as shear stress, pressure, and other mechanical factors that could damage the cell membrane. In addition, we must work in a sterile environment, so we must avoid elements that can hold bacteria or can generate cross-contamination (from one element to another).
Synthesis of the Bioprinting Process
In the printing process we normally find three phases: pre-printing, tissue printing, and post-printing. It is very important to understand each of them:
- Pre-printing
-
In this phase the main objective is to multiply the number of available cells obtained from a little biopsy. This is usually the bottleneck of the process, because despite presenting an exponential growth, we start with a very limited number of cells from the patient.
- Tissue printing
-
The deposition of the cells and the biological materials that will form the extracellular matrix as a suitable space to grow and develop. More materials can be added at this step to improve, for example, the mechanical properties of the scaffold.
- Post-printing
-
Or maturation of the printed tissues to prepare them for their normal function when implanted into the patient. This process has to also be carried out when used as alternative method, as some of the materials used have to degrade to be substituted by a new tissue.
During tissue printing, machines for cell culture (incubator, laminar flow cabinets, etc.) are required in order to culture and grow the cells. At post-printing, we will need also bioreactors, machines that simulate the physiological environment for each kind of cells and that allow the maturation of the tissues for their later introduction into the body. It’s important for muscle and bone tissues to be mature; otherwise they could collapse.
Conclusions
We are in a moment of history full of changes and revolutions at the social level, where citizen participation is increasing, even to fund and to carry out scientific projects. This is the perfect moment to create a more collaborative and scientific environment, to impulse potential technologies that can be used to advance in the field of medicine, as bioprinting, that is one of the technologies that may transform medicine as it is known now.
Bioprinting will become an indispensable tool in the field of personalized medicine, to patients with damaged organs or tissues, as it will allow to regenerate tissues from cells from the own patient.
Despite bioprinting is still a developing technology, new materials and methods are being published every day. We are sure that in a few years, the technology will be a routine technique at hospitals.
